Ultimate Guide to Intermittent Fasting While Breastfeeding
Medical Disclaimer: This article provides educational information only. Always consult your healthcare provider, lactation consultant, or registered dietitian before making dietary changes while breastfeeding.
Why Every New Mother Considers This Question
The postpartum period brings both joy and challenges. As a breastfeeding mother, you’re probably dealing with sleepless nights, hormonal changes, and wondering when you’ll feel like yourself again. Wanting to address postpartum weight gain is completely natural.

Intermittent fasting has become popular for weight management and metabolic health. But breastfeeding changes everything - what you eat directly affects your baby. The real question isn’t “Can I do intermittent fasting while breastfeeding?” but “How do I approach it safely?”
I’ll walk you through everything you need to know, based on current medical research and expert guidance, with both you and your baby’s health as the priority.
What Does the Medical Community Say About IF and Breastfeeding?
What Doctors Actually Say

Most doctors take a cautious approach to IF while breastfeeding. Unlike regular weight loss, breastfeeding adds a big complication - what you eat affects your milk and your baby’s growth.
The AAP says breastfeeding mothers need 450-500 extra calories daily [1]. The CDC recommends 330-400 extra calories for breastfeeding mothers [2]. Traditional IF usually cuts calories significantly.
La Leche League International, the go-to resource for breastfeeding support, recommends slow, careful changes to your diet while breastfeeding. They note that mothers need at least 1800 calories daily while breastfeeding to meet both maternal and infant needs [3]. You need to watch your milk supply and your baby’s growth closely.
Key Medical Considerations
Most healthcare providers consider these factors for IF while breastfeeding:
- Baby’s Age: Newborns (0-3 months) need frequent feeding
- Current Milk Supply: Established supply handles diet changes better
- Weight Loss Speed: More than 1-2 pounds per week isn’t recommended. JAMA explicitly states that intermittent fasting is not recommended for lactating women [4].
- Nutrient Focus: Maximize nutrients, don’t just cut calories
- Individualized Approach: There’s no one-size-fits-all answer - factors like baby’s age, mother’s health status, and current breastfeeding patterns all influence safety and appropriateness
Lactation Consultant Guidelines: Wait until milk supply is well-established (typically after 4-6 weeks, but often longer), start with conservative approaches (12-hour fasts maximum initially), and maintain adequate hydration throughout all fasting periods.
Dr. Sarah Johnson, a lactation consultant, notes: “The priority isn’t meal timing, but ensuring adequate calories and nutrients for mother’s recovery and baby’s growth.”
Understanding the Real Risks: What Every Mother Should Know
Milk Supply Concerns
The biggest worry with IF while breastfeeding is milk supply impact. Here’s what matters:
Immediate Risks:
- Under 1800 calories daily may decrease milk production. However, research shows that short-term fasting doesn’t necessarily impact milk macronutrients [5].
- Dehydration from fasting can reduce milk volume
- Nutrient deficiencies affect milk quality (especially vitamins A, D, B6, B12)
Watch Your Baby: These signs show your milk supply is adequate:
- Consistent weight gain
- 6-8 wet diapers daily
- Satisfied baby after feeding
- Regular bowel movements
Hormonal Considerations: Postpartum hormones already fluctuate significantly. IF may influence prolactin (milk production hormone), cortisol (stress hormones affecting let-down), and thyroid function. Monitor for any changes in milk supply or infant satisfaction.
Safe Intermittent Fasting Approaches for Breastfeeding Mothers
If you and your healthcare provider determine that intermittent fasting might be appropriate for your situation, some approaches carry significantly lower risk than others.
The Gradual Introduction Method
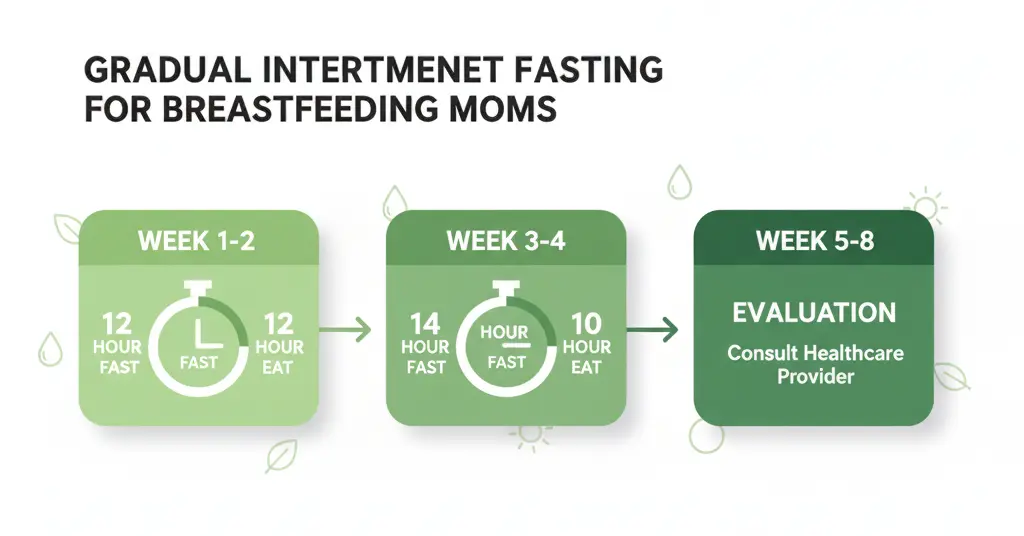
Week 1-2: Foundation Building Start with a simple 12-hour fast - essentially just extending your natural overnight fast. If you typically finish dinner at 8 PM, wait until 8 AM to eat breakfast. This approach:
- Allows your body to adjust gradually
- Maintains adequate calorie intake during eating windows
- Provides time to monitor milk supply and infant reactions
- Establishes baseline metrics for future adjustments
Week 3-4: Cautious Extension If all is going well, consider extending to 14-hour fasting windows. This might mean eating between 10 AM and 6 PM. During this phase:
- Pay close attention to hunger cues
- Ensure nutrient-dense meals during eating periods
- Continue monitoring baby’s satisfaction and growth
- Track your own energy levels and recovery
Week 5-8: Evaluation and Adjustment This is where many mothers find their sustainable balance. Some maintain 14-hour fasts, while others cautiously explore 16-hour protocols. The key is individualized assessment:
- Are you maintaining adequate calorie intake?
- Is your milk supply stable?
- How are your energy levels and mood?
- Is your baby thriving?
Nutrient Timing Strategies
When implementing IF while breastfeeding, when you eat becomes as important as what you eat:
Pre-Feeding Nutrition: Eating 30-60 minutes before breastfeeding sessions can help ensure optimal milk let-down and nutrient content.
Post-Feeding Recovery: A protein-rich meal after nursing sessions supports your body’s recovery and milk production for the next feeding.
Hydration Timing: While water intake should remain consistent throughout the day, focusing hydration around feeding times can support milk volume.
Strategic Calorie Distribution: Spread your nutrient intake strategically across eating windows to support consistent milk production. Don’t front-load calories to the point of being unable to eat later when baby might need to feed. Many breastfeeding mothers also benefit from continuing prenatal vitamins to fill potential nutritional gaps.
Using Tools for Safe Implementation
Proper planning and monitoring are crucial for success. Before starting any intermittent fasting protocol while breastfeeding, use our intermittent fasting calculator to determine appropriate eating windows based on your specific needs.
For establishing baseline health metrics, our BMR calculator can help you understand your starting point and set realistic goals. Remember, healthy weight loss during breastfeeding should be gradual - no more than 1-2 pounds per week.
As you progress, tracking body composition changes provides more insight than weight alone. Our body fat calculator can help you monitor fat loss while preserving the lean muscle mass essential for maintaining metabolism and energy levels.
Essential Monitoring: Keeping You and Baby Safe
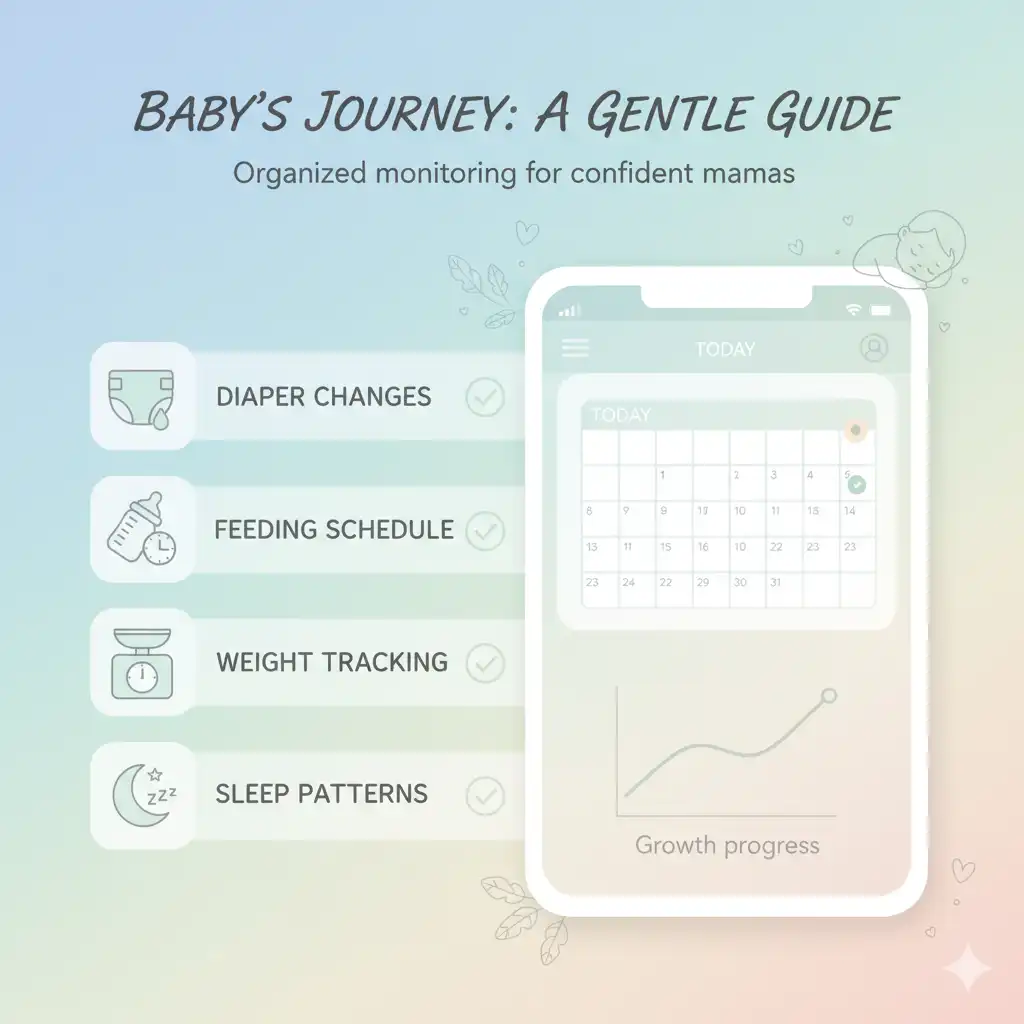
Daily Check-ins
Every breastfeeding mother practicing IF should establish a daily monitoring routine:
Baby Monitoring:
- Diaper output (6-8 wet diapers daily)
- Feeding behavior and satisfaction
- Sleep patterns and contentment
- Weight gain (weekly pediatrician visits for first few months)
Maternal Monitoring:
- Energy levels throughout the day
- Milk supply (let-down reflex, expressed milk amounts)
- Mood and emotional well-being
- Physical recovery from childbirth
Weekly Assessments
Set aside time each week to evaluate your progress:
Week 1-2 Focus:
- Is milk supply maintaining or increasing?
- Are you meeting your nutritional needs?
- How is your energy level compared to pre-IF?
- Is your baby gaining weight appropriately?
Week 3-4 Focus:
- Are you seeing positive physical changes?
- How is your sleep quality?
- Are you feeling deprived or satisfied?
- Has your healthcare provider noted any concerns?
When to Stop Immediately
Certain signs require immediate discontinuation of intermittent fasting while breastfeeding:
Infant Warning Signs:
- Sudden decrease in wet diaper output
- Poor weight gain or weight loss
- Increased fussiness or feeding difficulties
- Changes in sleep patterns or alertness
Maternal Warning Signs:
- Dizziness, lightheadedness, or fainting
- Rapid hair loss or brittle nails
- Extreme fatigue or mood changes
- Decreased milk supply
- Rapid weight loss (more than 2 pounds per week)
Listen to your body and your baby. No dietary approach is worth compromising their health and well-being.
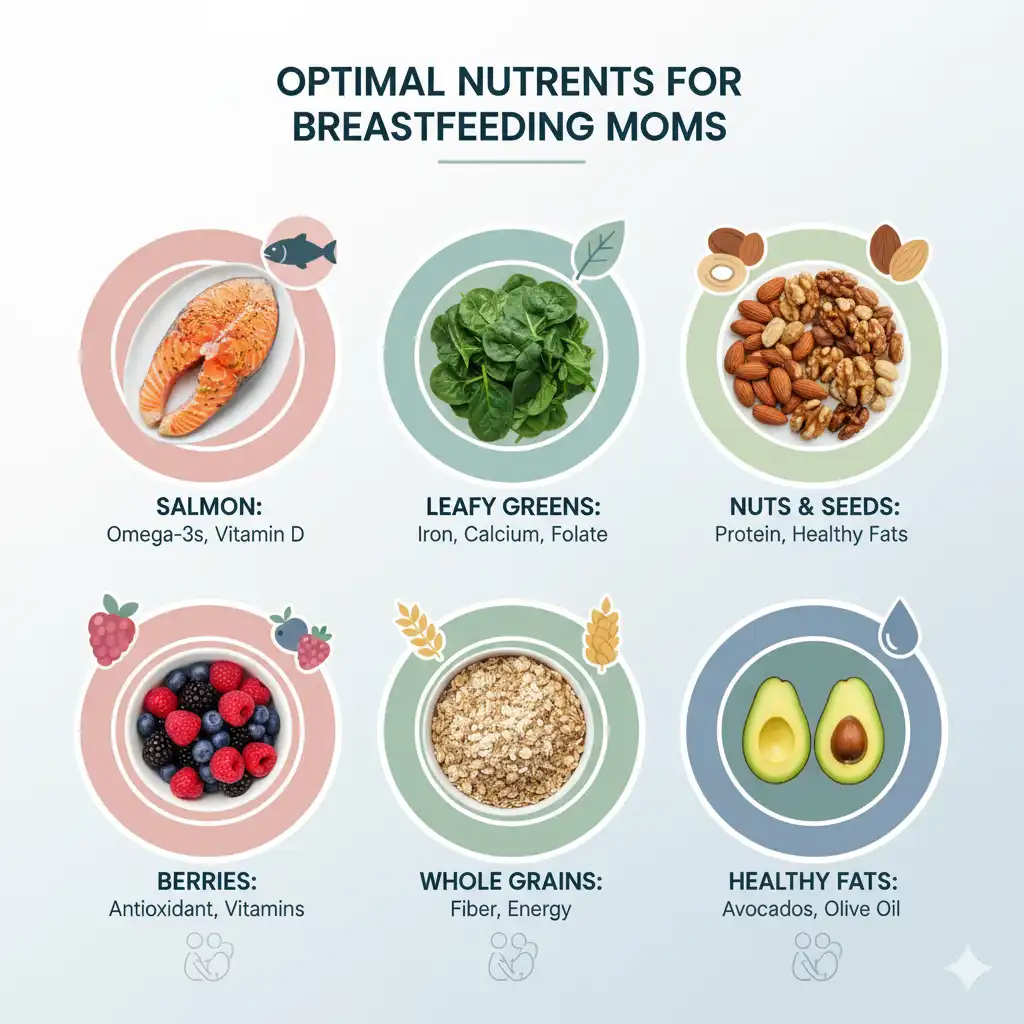
Nutritional Excellence: Maximizing Health in Eating Windows
When practicing intermittent fasting while breastfeeding, nutrient density becomes paramount. Your eating windows must pack maximum nutritional punch to support both your needs and your baby’s growth.
Protein Prioritization
Aim for 1.2-1.7g of protein per kg of body weight daily, distributed across your eating windows:
High-Quality Sources:
- Lean meats (chicken, turkey, lean beef)
- Fatty fish (salmon, sardines - excellent omega-3 sources)
- Eggs (complete protein with choline for baby’s brain development)
- Greek yogurt and cottage cheese
- Legumes and quinoa (plant-based complete proteins)
Strategic Timing:
- Include protein in every meal during eating windows
- Focus on protein-rich snacks between meals if needed
- Consider post-workout protein if exercising
Essential Micronutrients
Iron-Rich Foods (for postpartum recovery):
- Lean red meat, spinach, lentils, fortified cereals
- Pair with vitamin C sources to enhance absorption
Calcium Powerhouses (for bone health and milk production):
- Dairy products, leafy greens, almonds, sardines
- Consider supplementation if intake is insufficient
Healthy Fats (for baby’s brain development and maternal hormone balance):
- Avocado, nuts, seeds, olive oil
- Focus on omega-3 rich foods like salmon and walnuts
Meal Planning Examples
Sample Eating Window (12 PM - 8 PM):
12:30 PM (First Meal):
- Grilled salmon (6 oz) with quinoa and roasted vegetables
- Large mixed green salad with olive oil dressing
- Greek yogurt with berries
4:00 PM (Snack if needed):
- Apple with almond butter
- Small handful of nuts
7:00 PM (Final Meal):
- Lean chicken breast with sweet potato
- Steamed broccoli with lemon
- Small portion of whole grains
8:30 PM (Optional light snack):
- Herbal tea with a small piece of fruit if needed for satiety
Realistic Expectations: Benefits and Limitations
Potential Benefits (When Approached Safely)
Health Benefits:
- Improved insulin sensitivity and blood sugar regulation
- Reduced inflammation and enhanced cellular repair
- Gradual, sustainable weight loss while preserving muscle mass
- Better body composition and relationship with food
Lifestyle Benefits:
- Simplified meal planning and more structured eating
- Potential improvement in mindful eating and digestion
Important Limitations
Not a Quick Fix:
- Slower results than non-breastfeeding IF approaches
- Requires patience, consistency, and individual adaptation
- Success depends on your unique factors and metabolism
Requires Diligent Monitoring:
- Regular pediatrician check-ins and milk supply assessment
- Careful nutritional planning and ongoing attention to baby’s growth
May Not Be Appropriate For:
- Mothers of multiples or preterm infants
- Those with history of disordered eating
- Certain medical conditions or early postpartum period (first 6-8 weeks)
Special Considerations and Individual Factors
Infant Age and Development
Newborns (0-3 months): Most healthcare providers recommend avoiding IF during this critical period. Focus on establishing milk supply and bonding with your baby.
Infants (3-6 months): Some mothers may begin conservative approaches with close medical supervision. Milk supply is typically well-established, and feeding patterns may be more predictable.
Older Infants (6+ months): With the introduction of solid foods and more established feeding routines, IF may be more manageable for some mothers. However, nutritional needs remain high for continued breastfeeding.
Maternal Health Factors
Postpartum Recovery:
- Allow adequate time for physical healing (6-8 weeks minimum)
- Consider any complications from delivery
- Factor in sleep deprivation and recovery needs
Pre-existing Conditions:
- Diabetes or blood sugar regulation issues
- Thyroid conditions
- History of disordered eating
- Anemia or nutrient deficiencies
Current Lifestyle:
- Multiple children or high stress levels
- Irregular work schedules
- Limited support systems
- High physical activity levels
Creating Your Personalized IF Plan
Based on these considerations, here’s how to create a safe, personalized approach if you and your healthcare provider decide to proceed with intermittent fasting:
Step-by-Step Planning Process
Step 1: Medical Clearance
- Schedule appointments with your healthcare provider and lactation consultant
- Discuss your health history and current breastfeeding situation
- Establish baseline health metrics and goals
Step 2: Assessment and Planning
- Use our intermittent fasting calculator to create personalized eating windows
- Calculate your nutritional needs and establish monitoring protocols
Step 3: Gradual Implementation
- Start with 12-hour fasts (most conservative approach)
- Track food intake, energy levels, and breastfeeding patterns
- Schedule regular check-ins with healthcare providers
Step 4: Ongoing Evaluation
- Weekly assessments of both maternal and infant health
- Adjust protocols based on results and professional guidance
- Be prepared to modify or discontinue based on outcomes
Sample Progressive Timeline
Month 1: Foundation - 12-hour fasts, nutritional optimization, baseline metrics Month 2: Evaluation - Assess results, consider 14-hour fasts if appropriate Month 3: Optimization - Fine-tune approach for sustainable long-term pattern
The Bottom Line: Making an Informed Decision
Intermittent fasting while breastfeeding requires careful consideration, professional guidance, and diligent monitoring. When approached thoughtfully, it can be a safe and effective strategy for some mothers. However, it’s not appropriate for everyone, and the margin for error is smaller than when not breastfeeding.
Key Takeaways:
- Professional guidance is non-negotiable - never begin without consulting your healthcare team
- Gradual approaches are safest - start with conservative methods and progress slowly
- Monitoring is essential - track both your health and your baby’s growth closely
- Nutrient density trumps calorie restriction - focus on quality nutrition during eating windows
- Flexibility is crucial - be prepared to adjust or discontinue based on results
Remember: Your body is doing incredible work nourishing another human being. Any dietary approach must support, not compromise, this fundamental biological process. The goal isn’t just weight loss - it’s optimal health for both you and your baby.
If you decide intermittent fasting isn’t right for your breastfeeding journey, that’s perfectly okay. There are many paths to postpartum health and fitness. What matters most is finding an approach that supports your breastfeeding goals while honoring your body’s needs and your baby’s health.
Your health and your baby’s well-being are worth taking the slow, steady path to postpartum wellness.
Read More
Better to Skip Breakfast or Dinner in Intermittent Fasting?

Discover whether skipping breakfast or dinner works better for weight loss, energy, and health in your intermittent fasting routine
Read moreWhat are the basic rules for intermittent fasting?

Unlock your best self! Discover essential intermittent fasting rules to boost energy, weight loss, and simplify healthy living.
Read moreWhy is 16 hours the magic number for fasting?

Learn the science behind 16 : 8 intermittent fasting. Find out why a 16 hour fast boosts fat loss, improves metabolism, and supports longevity.
Read more